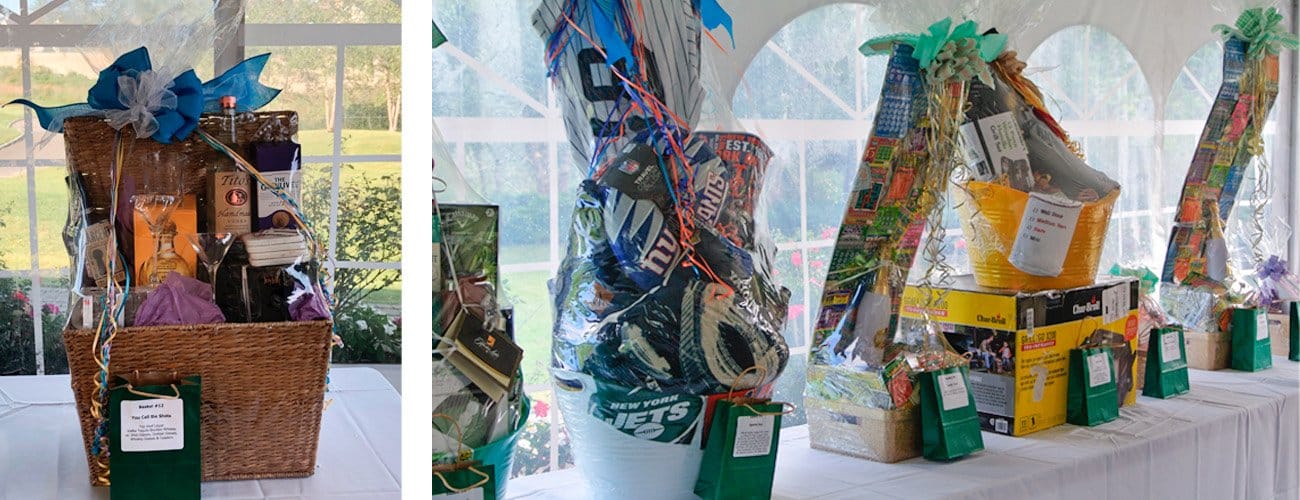
Your help is vital in ensuring that we continue to fulfill our mission of exceptional care.
About Us
History
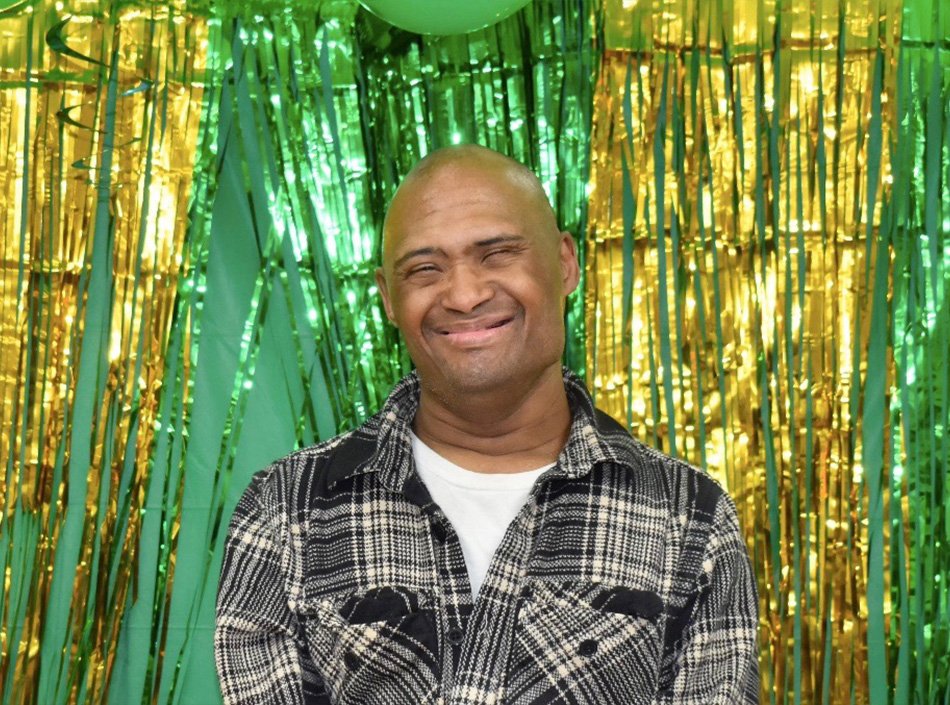
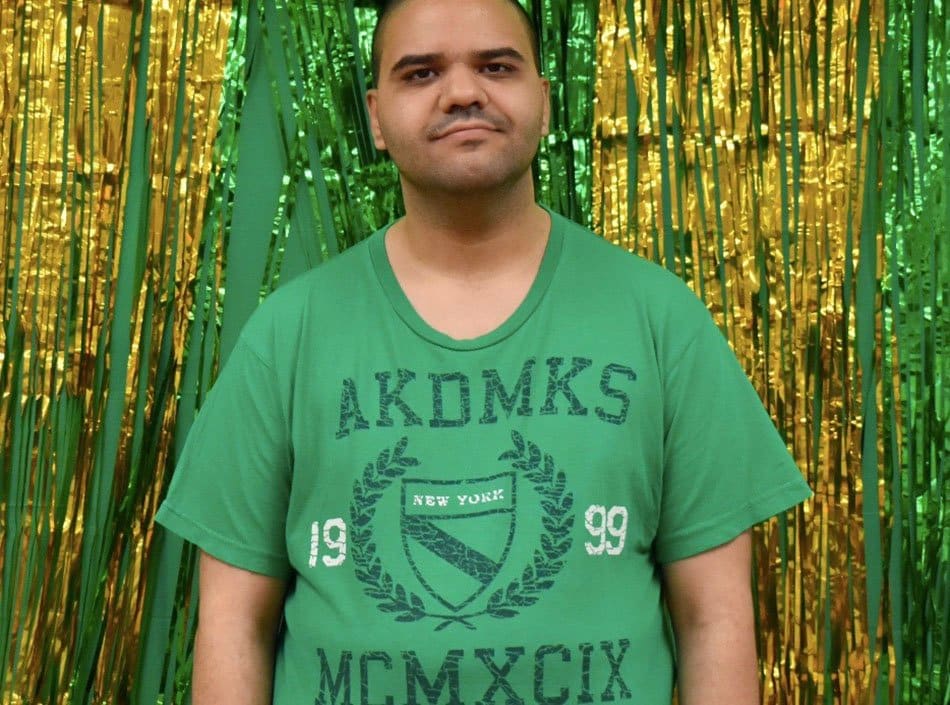
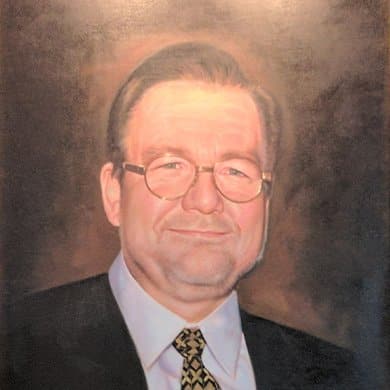
When we opened our doors in 1985 under the direction of the late John P. Welch, ILA created a residential haven for people whose only other means of long-term care was in large institutions. Mr. Welch’s credo was, “ILA will be their home for the rest of their lives.”
Through the advocacy of our compassionate, hard-working staff and with the support of the New York State Office for People With Developmental Disabilities (OPWDD), ILA is committed to fulfilling Mr. Welch’s legacy. As we grow, so do our Individuals, as they continue to flourish and lead bright, fulfilling lives in the community.
“
I can’t say enough good things about ILA’s staff.”
– Eileen N., Mother of ILA Individual
30 Years
of ILA
Governance

Our Policy
It is the policy of Independent Living Association, Inc., ILA Case Management Services, Inc. and the New York State Office for People with Developmental Disabilities (OPWDD) to assist in ensuring the integrity of the Medicaid program by safeguarding against Medicaid abuse and the submission of fraudulent Medicaid claims.
OPWDD acts under the direction of the New York State Office of the Medicaid Inspector General (OMIG) to identify inappropriate Medicaid claims and to maintain Medicaid program integrity.
The OMIG has been established by statute as an independent entity within the New York State Department of Health to improve and preserve the integrity of the Medicaid program by conducting and coordinating fraud, waste and abuse control activities for all State agencies responsible for services funded by Medicaid. In carrying out its mission, the OMIG conducts and supervises all prevention, detection, audit and investigation efforts with OPWDD and other State agencies. ILA & ILA CMS are committed to adhering to the principles of good governance.
Corporate Compliance
In accordance with the OMIG, ILA has developed policies and procedures to ensure that our organization is in compliance with required Medicaid statutes:
If fraud, waste or abuse has been witnessed, please contact the ILA Corporate Compliance Officer, Teako Lewis, at 718-858-1204 or [email protected]. All reports will be confidential.
Privacy Practices –
Health Insurance Portability & Accountability Act (HIPAA)
Jonathan’s Law
The law is the result of the efforts by Michael and Lisa Carey. The tragic death of their 13 year-old autistic son, Jonathan, raised awareness of the need to provide parents and guardians with timely information about incidents affecting the health and safety of their children in residential care facilities. Michael and Lisa Carey were unable to access records regarding their son’s care at a private school for developmentally disabled children in 2004. They had become tireless advocates for changing the law governing the disclosure of such records.
The culmination of their efforts was Jonathan’s Law, which is a combination of two state laws that expand access to records related to incidents and allegations involving individuals residing in residential mental hygiene facilities, including, in certain circumstances, records related to incidents that occurred prior to the enactment of these laws.
Jonathan’s Law A.6846-A:
- Requires telephone notification to parents of any reportable incident within 24 hours of the incident.
- Ensures that all incidents are reported to parents.
- Parent receives a copy of the written incident report upon request (names of individuals involved are not included).
- Parents, upon written request, are entitled to a copy of investigative reports about patient abuse or mistreatment. Names of individuals involved are not included.
- Commission on Quality Care and Advocacy for Persons with Disabilities is required to develop and distribute a pamphlet regarding the rights of parents to receive records and the process to appeal the denial of such request.
- Incident reporting requirements now include all licensed and certified facilities providing services to persons with mental disabilities.
- Task Force is created to identify records, review provisions and seek means to improve practices.
- Commissioner of OPWDD can impose a fine of $1,000 per day or maximum of $15,000 per violation on an OPWDD facility that is not in compliance.